Dear Rae: How to Choose the Best Addiction Treatment Center?
Dear Rae:
My wife’s addiction and mental health issues have gotten out of hand. It is impacting our quality of life, and our children’s lives. But I am overwhelmed by the options for treatment. How do I find the best addiction treatment center for her? How do I know what she needs? We would like to find something near where we live. Is there a list of things I should look for?
TJ
Dear TJ:
Choosing a drug and alcohol treatment center for a loved one (or yourself) can be an overwhelming process. Unfortunately, there are unethical organizations in the mental health field who can cause the selection process to be unnecessarily confusing. These days, it is important to research the options. Arm yourself with the right questions to ask when you call a treatment center. At Sanford Behavioral Health, our admissions team spends time answering all of your questions.
Warning Signs
If the person on the end of the line is abrupt, pushy, or wants to send you far from home without a good reason, hang up. Also, look out for programs that offer to pay for your plane tickets or travel. Also those who say they will waive all deductibles, coinsurance, and out of pocket costs, or offer to pay for your insurance coverage. If it seems too good to be true, it is.
And Questions to Ask and Important Information to Gather Before you Decide
Where Are You Located?
This is no time for a runaround, so ask for a specific location. Respected rehabs should be transparent. Sanford Behavioral Health is located in five beautiful facilities in Greater Grand Rapids, Michigan. We treat patients living in Michigan and beyond.
What are Your Accreditations, Credentials and Licenses?
Reputable treatment centers are licensed by the state and are accredited by the Commission on Accreditation of Rehabilitation Facilities (CARF) or The Joint Commission. Both base criteria on industry performance standards. Similarly, LegitScript certifies rigorously vetted facilities to advertise on Google and Facebook, which provides consumer protection. Look for marks of distinction displayed on websites.
Do You Have a Multidisciplinary Team? What are Their Credentials and Licenses?
Clinical and medical staff must meet nationally recognized standards for professional practice. Consequently, make sure to ask about training and staff experience, medical depth, and clinical credentials. The team should include:
- On-site psychiatrists and medical doctors
- Medication management and medication-assisted treatment (MAT)
- Advance practice providers with addiction and psychiatric specialties
- RNs, registered dietitians
- Master’s level and above clinicians
- Case managers, peer recovery coaches, recreation therapists, and administrative staff.
Do You Have Mental Health/Co-Occurring Services?
More often than not (about 85% of the time at Sanford) addiction and eating disorders come with complicating factors such as depression, anxiety or trauma known as co-occurring disorders. In fact, up to 35% of those with a substance use disorder also have an eating disorder (NEDA).
What About Evidence-Based Practices? Individualized Treatment?
Evidence-based means therapies are effective, science-based and proven.. At Sanford we use cognitive-behavioral therapy, dialectical-behavior therapy, experiential therapy, emotion-focused family therapy, seeking safety, acceptance and commitment therapy, and more. Additionally, we offer individual, group, or family therapy throughout the treatment process. Of course, we use person-centered, highly attuned therapeutic interventions in all our programs at Sanford.
Do You Have a Full Continuum of Care? Does it Include a Family Program?
The term “continuum of care” means the delivery of care over a period of time. This means connecting individuals to the various parts of the continuum, based on the assessed needs, at any given point in the recovery process. At Sanford, our continuum includes assessment, detox, residential treatment, PHP, IOP and outpatient services. We include family in our signature Family Program. We also provide long-term support for alumni and families.
Are There Extracurricular Activities?
Boring treatment, or treatment isolated from the “real world” is not as effective as treatment that incorporates snippets of real life in the safety of treatment. At Sanford, we include experiential therapy into the recovery process whenever possible. Experiential therapy utilizes recreation, creative expression, and other activity-based techniques and excursions to restore physical and psychological health.
Can You Tell Me About Your Outcome Data/Success Rates?
Ask about the treatment center’s research-based methods for tracking outcome data. Similarly, ask them to define “success”,
Last But Not Least, What Insurance Do You Take?
The cost of addiction treatment is an expense most individuals have never planned or budgeted for. So, look for rehab facilities that are in-network with your insurance. Today Sanford has fifteen in-network insurance contracts and many initiatives in the works.
Research and Discuss
TJ, as you conduct your own careful research and discuss recommendations with professionals and friends you will feel confident making a decision about treatment. Perhaps presenting several options will help your wife feel that she has some input in the decision. Be sure to encourage family involvement in both the search process and the treatment process. And most of all, try not to get discouraged. There is a program out there suited to your family’s needs, ready to help your wife begin her treatment journey.
Dear Rae: How do I Talk to My Spouse About Their Drinking?

Find a time when you are alone and he has not been drinking, is overly tired or visibly stressed
Dear Rae:
I’ll get right to the point – since the pandemic began, my husband has been using alcohol as a crutch. In other words, he drinks to reduce his stress, but it actually adds to the stress in our home. Now that the world is opening back up again, he is still drinking every evening (sometimes starting at lunchtime). It is definitely impacting our relationship, because when he drinks he either becomes sleepy and doesn’t want to do anything or he gets argumentative for no reason. I do not understand why he is doing this to our family. It feels like he has chosen alcohol over us. I have two small children and I think they can tell there is “something wrong with Daddy”. Rae, how do I talk to him about my concerns without it turning into another fight?
Carol L.
Dear Carol L:
First, let me start by saying you are not alone. Stress goes hand-in-hand with increased drinking, and statistics show that stress, anxiety, and alcohol consumption skyrocketed during the pandemic. The comorbidity (taking place at the same time) of anxiety disorders and alcohol misuse is a common occurrence. And once anxiety and alcohol misuse co-occurs, they feed each other. Stress causes an individual to drink and drinking causes stress. Also, the cycle often progresses if left untreated, so it is a positive that you have recognized a problem and are ready to get help. Unsure if your husband’s drinking has progressed to alcoholism? A rule of thumb is – if a family member’s drinking is negatively impacting the family, there is a drinking problem.
Your husband’s anger or avoidance by sleeping might be because he feels embarrassed, ashamed, or threatened. Especially if his alcohol use has progressed to dependence. Approach him with sympathy and kindness, and without judgement. Find a time when you are alone and he has not been drinking, is overly tired or visibly stressed. And let him know how his drinking has affected you and your family. Offer suggestions and support.
Things to Avoid when Talking to a Loved One About Their Drinking:
- Choose a time when your loved one has not been drinking or is drunk
- This is a frustrating and hurtful situation, but do not approach him with anger, sarcasm or talk down to your husband about his drinking
- Do not argue – if it begins to get heated, walk away
- Do not blame
- Don’t make excuses for him
- And last but not least, do not put this off. You have a better opportunity for success in recovery if you catch the problem at misuse and treat it with a medical model.
Getting Help for your Loved One
Fortunately, several evidence-based strategies are available for treating anxiety and alcohol use disorders, including both pharmacotherapy and psychotherapy approaches. Your best friends are research and education. Look for treatment centers in your area that offer integrated programs treating both disorders. There is a wealth of options for care including: residential, day programs, intensive outpatient programs, one-on-one therapy, family therapy, and support groups.
Most of all, don’t give up. This disease wears everyone out, not just the person who is drinking or using. The brain problems associated with substance use disorders dramatically hinder a person’s ability to make the right decisions and your husband’s poor choices are likely reflective of an escalating progressive disease. Seek out family programs and supports to reassure yourself you are not alone. And remember – when your husband gets well, the entire family gets well.
.
Dear Rae: He Drinks Way More Than I Thought!
Dear Rae:
I am embarrassed to say I met a guy 3 years ago online and I fell in love. Yes, he drank, but I was not aware of the degree. Trust is an issue with me, but I tried to be open. We married 2 years ago, and he moved us away from everything I knew – family and friends. And he manipulated my money right out of my hands. Now I’m all the way across the country, and I know no one. We have been in our new home not even one year, and he incessantly lies and drinks way more than I thought. When he gets really drunk, he kicks me out. It has happened several times, he says he does not need me or the drama. I have no family, I am on a fixed income and scared.
PC
Dear PC:
I am so sorry you are going through this. It is not surprising that you feel isolated and afraid. Addiction and isolation go hand in hand. And your husband’s alcohol misuse, is causing him to want to be alone with his addiction. It is why he “kicks you out”. That way he can avoid conflict, hide his shame, and allow his alcohol use to run the show. Addiction is a disease, and it affects both the brain, and the behavior.
Living away from loved ones, and the COVID-19 pandemic is even more reason for you to self-advocate in this situation. I’m sure it feels impossible, but there are some things you can do to protect yourself. First, if you are in danger, you should call a local hotline, or local authorities. If you have family/friends who live away from you, rekindle relationships, call, text, email, or zoom and share your situation. Ask for help if you can.
If it is safe to do so, talk to your husband when he is not under the influence of alcohol and address the problems in your marriage calmly. There are always free, local organizations that can help you and your husband manage his drinking. If he is not willing to go to a meeting, Al-Anon is an organization for those who are worried about someone else’s drinking. Al-Anon will help you to determine patterns of behavior, triggers to his drinking, and provide coping skills for you.
Focus on your personal needs …
The family collapse, resulting despair and inability to “fix” out of control behavior, has likely begun to pervade all of your life’s activities. The general pattern for those living with addiction in the home is to take on additional responsibilities in an attempt to control dysfunctional behavior. These efforts are sincere, but do not make the situation any better.
The only way to begin to emerge from this cycle is make a concerted effort to focus on YOUR personal needs. Let go of the embarrassment, this is not your fault. Seek out a community or support system that
understands your situation. Only when you implement self-care will you begin to overcome the fear and feel empowered. Remember, it’s his disease that is lying and if you begin to lose your resolve his disease will remain in the driver’s seat.
Dear Rae: Should We Delay Treatment for our Son?

Start with active listening and acknowledgement that everyone struggles sometimes.
Dear Rae: Since March, our 21-year old son has been showing signs of alcohol and marijuana addiction. He is always sneaking off in our back yard, and there have been many times when he has been staggeringly drunk or high. I guess we are seeing it now that we are all together at home and he is “going to college” online. But it seems to be worsening, and he’s barely speaking to us. My question is, should we wait till things calm down with COVID-19 to get him help? Nancy B.
Dear Nancy B.:
First, let me say you are not the only one to feel the impact of COVID-19 on the family system. The close quarters shine a light on negative behaviors you might not have seen before. And the boredom, anxiety, and uncertainty of these times are the perfect recipe for self-medicating with drugs and alcohol. It is also not surprising that you are concerned about your son’s safety.
It seems, even though he is completing courses online, your son has time on his hands. One of the things we recommend to our clients at Sanford, especially during a pandemic, is that they establish connection and accountability. It is also important for your son to recognize that 2020 is a challenge for everyone and a schedule of meaningful activities is key to good mental health.
Easier said than done? Especially with a non-compliant, silent young adult? That brings me to your question about waiting to get help. The answer is: do not wait. Talk to your son about your concerns, if you have not already done so. Pick up the phone and talk to a professional. The rise in alcohol sales, and the increase in every marker charting substance misuse and mental illness, tells us that COVID-19 is wreaking havoc on peoples’ well-being.
Options for Safe Treatment
There are a myriad of options available to you and your son. At Sanford, residential treatment is in-person and safe. Some clients say they feel safer in our houses than in the “outside world”. If you would like to explore outpatient options such as Intensive Outpatient Programs, educational classes, or outpatient therapy, telehealth is a good option for your son at this time.
Simply put, telehealth uses “video chat” technology to offer the same evidence-based practices that in-person addiction programs provide, but in the comfort and safety of home. It would give you and your son access to information about substance misuse, provide community, and help to impose a well needed structure to his life. You would have the benefit of virtual attendance with the family telehealth groups.
There is no “good time” to confront drug or alcohol misuse. And during COVID-19, it might seem easier to let things slide for a better time, but waiting is not wise. Start with active listening and acknowledgement that everyone struggles sometimes. To keep the conversation productive, do your best to have an open mind and hear your son’s point of view; remain calm and relaxed. Talk to him about why he is drinking and using marijuana and prompt him to think about his future. This may provide insight into what’s underlying his desire to use and help manage his motivations. Finally, discuss and agree on consequences and help him understand legal implications. Talk about the risks associated with Substance Use Disorder just as you would any disease. Keep your pulse on how he is coping and if the struggles continue, seek professional help.
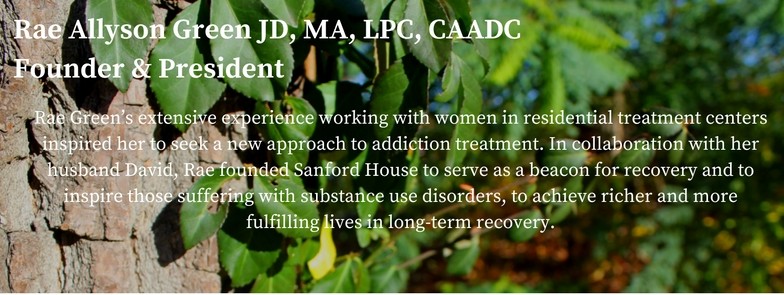
Rae Green, JD, LPC, CAADC
To ask your own questions of Rae, click the link below:
Dear Rae: Is My High Anxiety Threatening My Recovery?
Dear Rae: I’m home alone and scared – is my high anxiety threatening my recovery?
I am reading everywhere that this difficult time is particularly hard on those of us in recovery. I am a year sober from alcohol and drugs myself, live with my boyfriend and I am really struggling with anxiety. I’m working from home, but he is still working in the outside world. I feel confused about what to do to stay safe. I keep thinking of what would happen if I got sick. What if I had to go to the hospital? What if I lose my job? And what happens if my boyfriend gets coronavirus? I am having trouble sleeping and to be honest, I have been thinking of drinking. My boyfriend does have beer in the house … What can I do to get my anxiety under control?
Carol R.
Dear Carol R.
High anxiety during this time of physical and social distancing is understandable. For those in recovery, it is a particularly difficult time, as the treatment of substance use disorders (SUD) and recovery incorporates group therapy and connection in 12-step groups and other community activities. Counselors and therapists understand the significance of personal connection, and now that 12 step meetings and in-person sessions have ceased, it’s critical to seek out connection via online video conferencing platforms. Or even an old-fashioned phone chat! It’s way easier for those with a history of substance use disorder to fall back into isolation. Your situation is further exacerbated by two things: you are staying at home, seemingly worried about your work stability, and your boyfriend is still drinking.
Anxiety and SUDs go hand in hand. In fact, there is a prevalence of substance use disorders among those with anxiety disorders. Often, that is because alcohol and drugs are used to ease tension. It sounds like your anxiety could be related to our current state of unpredictability, as our normal routines have been interrupted by uncertainty and fear. But as a person in recovery, you already know that alcohol and drugs are not an option for you.
Things to do to reduce high anxiety
Slow down – take stock
Be grateful for all that you do have. Maybe even spend some time writing these things down. For example, What are 5 things you are grateful for right now?
Create control for yourself
Challenge your thoughts. Many things in life are beyond our control. Focus on the things you can control such as the way you choose to react to problems. Do your best at your work, and follow coronavirus guidelines.
Talk with family members about their drinking or drug use …
Let your boyfriend know the effect his drinking is having on your stress level and your recovery. If your boyfriend is a problem drinker, It can be hard to bring up the subject, but try to keep the lines of communication open and offer support. And if you are feeling vulnerable it is never appropriate to have alcohol in the house when you are there alone.
Limit television and social media
With the world in a state of crisis, gathering information is one way to feel in control. But over-consuming the news, especially fearful and unpredictable news, will not do your mental state any favors.
Stop thinking and take a walk
When you’re experiencing anxiety, the last thing you probably feel like doing is getting up and moving. But physical activity is a huge stress reliever—and you don’t have to be an athlete or spend hours exercising to experience the benefits. Movement releases “feel good” endorphins and it serves as a distraction from your daily worries.
Open the windows
The sensory stimulation provided by fresh air, along with the sound of nature, has been shown to increase brain activity, which can help to relieve anxiety and depression.
Meditate
The fastest way to reduce stress is by taking a deep breath and focus on your surrounding with your senses (what do you see or hear?). Perhaps look at a favorite photo, smell something delicious, listen to a favorite song, or hug your pet if you have one. These things can help you quickly relax and focus yourself. The best way to “get better” at meditation is to practice it daily. Close your eyes and recite a positive affirmation.
Work, eat and sleep in different locations
By now, deep in the coronavirus quarantine, many of us are trapped in an even more extreme cycle of “eat, sleep, work, repeat.” Try to change up the scenery.
Live in the day/moment – no catastrophic thinking
“The secret of health for both mind and body is not to mourn for the past, worry about the future, or anticipate troubles, but to live in the present moment wisely and earnestly.” – Buddha
Try to stop the “what ifs” by taking precautions
When facing major challenges, try to look at them as opportunities for personal growth. Try to view this stressful situation from a more positive perspective. And if you fear you or your boyfriend are vulnerable to coronavirus, strictly follow guidelines for protection and decontamination.
Virtual Relapse Prevention Classes, 12-step virtual meetings
Humans are intensely social beings and need to feel connected, particularly in recovery. Personal sharing is one of the easiest and most overlooked ways to create that connection, and there are endless options for online venues in which to do this. Attendance at virtual meetings is not dictated by geography. Try a meeting out of state – a new experience to embrace.
This too shall pass …
I want to remind you that you have experienced an entire year in recovery. Take a moment to think about what the pandemic would be like to navigate if you were still drinking or using. You have already met incredible challenges. Now is the time to rely on those coping skills you have honed during a year of recovery. If you are used to going to 12-step meetings, find a virtual option. Garden, learn to knit, read, or get out for a run. This difficult season will pass, but your hard won recovery will be with you for a lifetime!
Rae Green, JD, LPC, CAADC
To ask your own question of Rae, click the link below:
Dear Rae: Will Holiday Temptations Derail my Recovery?

Dear Rae: I am 92 days drug and alcohol free. How do I manage my recovery during the upcoming holiday season? There are so many temptations! Emily
Dear Emily:
First, congratulations on 92 days. I am glad you’ve written to me and that you have a healthy respect for the challenges the holidays bring for someone who is new to recovery.
The season is meant to be a time for joy and merriment …
But there is no question this time of year brings additional temptations. It seems like the holidays put demands on everyone to be present and “festive”. Drinking is at a maximum at work events, family dinners and neighborhood parties. Traveling adds additional stress. And the need to host the “perfect” party or find the “ideal” gift for loved ones takes precedence over self-care.
There are cocktail parties (even the name is triggering) and drink-heavy gatherings can bring about strong urges. BUT, you don’t need those old substances to have a festive time. There are some proactive steps you can take to reduce your stress and keep moving forward in your recovery.
Bump Up your Support System
During the holidays, reach out to your sponsor, therapist, and support groups more frequently. And spend time with others in recovery. Your support system can help you recognize your personal limits. Talk with sober pals before you go to that holiday party and plan to meet with them afterwards.
Have a Plan in Advance
If you are going to a party where there will be alcohol or other substances, evaluate the situation. Have a plan in advance or consider not going this year. If you decide to attend, bring a sober friend with you. Drive yourself so you can make a quick exit, and won’t have to wait for a ride. Also, you can arrive early and leave early to avoid prolonged exposure. Or, you can set a timeframe beforehand and clearly state your intentions when you arrive. The holidays are the time to establish healthy boundaries.

The new ritual of hot chocolate in front of the fire!
Prepare Responses and Rehearse Them
If you’re not ready to share your recovery with family and friends, have a strategy for turning down drinks or other substances, as this is when vulnerability is at its peak.
Know your Triggers and how to Manage Them
Take care of your mental and physical health. Be sure to set aside quiet time each day. Fit relaxation and meditation into your day, even a few minutes, no matter how busy you are. Get enough sleep every night too. Eat nutritious meals or a snack every few hours to keep your blood sugar up. Low blood sugar can make you feel anxious or irritable – increasing the risk of impulsive behavior. As a person who is new to recovery, stay in low risk situations and avoid ones that are high risk. When you are further along in recovery, know your plan for when you’ll be in a medium or high risk.
Celebrate the season in a new way. Create new rituals or symbols that help redefine joy for you in your recovery during the holidays. You can host your own holiday party for recovery friends or your support group. This is a festive time of year to embrace the joy of a restored life, nourish your spirit, and offer the gift of service to others. You have already given yourself and your loved ones something to celebrate — your best self.
Dear Rae: What’s Dual Diagnosis? Is That What I Have?

Dear Rae: I am researching rehabs for my depression, and I also have a drinking problem. I keep reading about dual diagnosis and co-occurring disorders. Is that what I have? N.K.
Dear N.K.
“Dual diagnosis” and “co-occurring disorders” are both terms that refer to someone who experiences a mental illness and a substance use disorder (SUD) simultaneously. Either disorder, SUD or mental illness, can develop initially and even cause the other disorder to develop or worsen.
Dual Diagnosis and Co-Occurring Disorders …
You are not alone. Some of the most common co-occurring mental health disorders found in those with SUDs are mood and anxiety disorders. These include depression and bi-polar disorders (mood related), and post-traumatic stress disorder (PTSD) and trauma (anxiety related). In fact, about 20 percent of Americans with an anxiety or mood disorder also have a substance use disorder. And about 20 percent of those with a substance use problem also have a mood disorder, depression or other mental health challenges.
When high anxiety strikes, you might self-medicate with alcohol to ease the pain. Self-medication is common and defined by the use of drugs or other substances to treat self-recognized or self-diagnosed mental health issues.The substance may feel like it’s helping at first, but it’s a vicious cycle, not an end solution.
What’s more, those who have experienced PTSD and trauma can have a lower than normal baseline of dopamine. This makes them more susceptible to substance use, misuse and dependence because the substance creates a feeling of “normalcy.”
Treatment for Dual Diagnosis
Now, to answer your question: Is that what I have? A more thorough assessment would have to be performed. An assessment is used to diagnose and develop specific treatment recommendations. And a co-occurring disorder can be difficult to diagnose, because symptoms of substance dependence can mask symptoms of mental illness.
But, the best treatment for dual diagnosis is an “integrated intervention”. This means you would receive care for both your diagnosed mental illness and SUD at the same time. Treatment is not the same for everyone. Individualized treatment includes detoxification; residential or intensive outpatient treatment; recovery support; psychotherapy; and medication can also be used as a tool.
You would be advised to seek help form a reputable therapist or addiction treatment center – specializing in working with co-occurring disorders. At Sanford, we treat the whole person in a comprehensive approach to wellness and recovery – addressing co-occurring conditions in one location (this is still an exception in most treatment settings). Research by the National Institute on Health states that an integrated approach will improve patient outcomes. Better outcomes include reduced substance use; decrease in legal and medical costs; improved mental health symptoms; job and relationship stability; and improved quality of life.
Think of this as a time for learning skills and receiving education rather than “fixing” something. We live in an idealized society and there can be a sense of shame for not feeling emotionally healthy. But seeking help in the form of therapy or treatment is not a sign of weakness. Rather a proactive indicator of strength to come.
Rae Green, JD, LPC, CAADC
To ask Rae a question click here:

I Went To Detox – Do I Still Need Treatment Dear Rae?

Dear Rae: I just got out of Detox and I feel pretty solid. Do I still need to go to an addiction treatment program? L.J.
Dear L.J:
In a word, yes. You need some type of addiction treatment program or intensive therapy after a stay in a detox unit. The purpose of detox is to rid the body of alcohol or drugs in a physically safe way. You are feeling “solid” because you have been medically stablized. And you are probably feeling relieved that you are getting professional help. But detox is not treatment. Think of it as the first step to getting well.
What is Detox?
Not everyone who goes into treatment needs to go to a detox unit. But in some cases medical stabilization is necessary to safely admit someone into an addiction treatment program. Factors that play into the need for detoxification include: the amount, frequency and duration of substance use. It also depends on your drug of choice. At Sanford Addiction Treatment Centers we make these determinations at the initial Screening and Assessment.
Detox addresses the physical aspect of addiction. Treatment addresses the emotional pain that underlies substance use.
In fact, it is important to go straight from the detox unit to some type of program. Here’s why – withdrawal from addictive substances reduces tolerance. And if you’ve been through detox, you can become effected more quickly and intensely by your substance of choice. You are at risk of overdose. Do not be fooled by how good you are feeling at the moment – there are emotional triggers and cravings ahead. And without the proper tools to address these bumps in the road, you are vulnerable to relapse.
Options for addiction treatment:
There are many options for addiction treatment. From working with an individual therapist who is qualified in treating addiction to a lengthy stay in a residential treatment center. There are also Intensive Outpatient Programs (IOP), full-day programs and classes in relapse prevention, early recovery and mindfulness that neccessitate different levels of care. Sanford admissions and assessments help determine what might be the best or most appropriate fit.

Just the beginning of life in recovery…
Detox is not the end of the story, rather the beginning. Your body has been stabilized, but both your mind and body still have healing to do. The fact that you are feeling “solid” now does not mean you can simply resume everyday life because you are now sober. This is the time to learn coping strategies to deal with the inevitable cravings. And treatment/therapy will help equip you to deal with the normal stresses of everyday life – free of addictive substances
Rae Green
Dear Rae: I Relapsed. How Do I Move Forward?

Dear Rae:
I am (or was) a recovering alcoholic. I have been sober for three years. Yesterday, it was raining and gray and my husband was out of town on business. For some reason I went to the liquor store and bought a bottle of vodka. I didn’t really even think about it – it was like a dream. I drank most of the bottle in an afternoon. And when my husband called he accused me of being drunk. I lied and said I wasn’t, but he didn’t believe me. We got in an argument and he hung up on me. I am sitting here now wondering what to do. Feeling sick that I relapsed. I am terrified the whole mess is going to start over again. Rae, how do I move forward from this? K. D.
Dear Recovering K.D.:
First, let me say you can move forward from this. In fact, sitting in the feeling you describe will perpetuate your sense of failure and guilt. So, let’s get back on track. The American Society of Addiction Medicine (ASAM) defines addiction as , “A primary, chronic disease of brain reward, motivation, memory and related circuitry.” The ASAM adds, “Like other chronic diseases, addiction often involves cycles of relapse and remission.” As to feeling like it was a dream, the nature of this disease can block recognition of the warning signs or even signal a need to use. Triggers like dismal weather or isolation can be negative influencers.
Time to get back to your recovery …
This is not an excuse, but it is something to remember as you pick yourself up and get back to your recovery. If you have anything left in the bottle of vodka, pour it out. And when your husband gets home it is a good idea to tell him you relapsed and that you are sorry you lied. Your family can be your best allies, but only if you put your trust in them.
There are warning signs before a relapse. And a lapse usually means your recovery plan is in need of some tweeking. You don’t say whether you have children or work outside of the home, but it is always important to be accountable to someone or something. It is time to up your recovery game and include your husband or other loved ones in the process. If your family is educated about the disease of addiction they can help you be vigilent.
A wise man once said, “Recovery is like going up a down escalator. You must keep moving forward.” Now is the time to find a Relapse Prevention class or consider an Intensive Outpatient Program to help you develop the tools to manage the disease.
Rae Green, JD, LPC, CAADC

Dear Rae: Why Can My Boyfriend Drink More than Me?
Dear Rae:
I am a currently a Junior and I have been drinking heavily for my entire time at college. Mostly beer, but we also do shots. Lately, after a night of partying, my hangovers seem to be getting worse. If I’m honest, I don’t feel that great most of the time… but it doesn’t seem to stop me from drinking again when my group gets together. My boyfriend, who is about my size and weight, seems to be able to drink a lot more than me without the same negative result. And he and his friends are always the ones who instigate our drinking. Although I think about drinking all the time. It’s weird because I can do most things better than him. Is there a difference between men’s and women’s alcohol tolerance? This whole thing has me a bit worried. KD
Dear KD:
Let’s start with your question. Yes there is a difference between men’s and women’s tolerance to alcohol. There are many reasons for this. Women have less water in their bodies so there’s a higher alcohol content in their bloodstream than men. Even if they drink the same amount. It’s why women black out more than men. Women are also more susceptible to heart disease, liver damage, complications with procreation and breast cancer as a result of drinking.

And that’s not all. You say you “think about drinking all the time”. And that you drink even when you are feeling ill or hungover. So let me caution you on something else – women develop substance use disorders in less time than men – it’s called telescoping. And there has been a rise in women’s alcoholism in the past 10 years. For the very reason you say is “weird” – women can do everything men can do. Get better grades; succeed at a stressful career; manage child rearing and work outside of the home; participate in extreme sports. But women can’t drink like men.
The worry and self-observations you express about your alcohol consumption are insightful and courageous. I encourage you to take serious note of the negative consequences, allow yourself the opportunity to accept the logic in quitting and embrace the beauty of sobriety. Before it escalates into a physical and emotional crisis.
Dear Rae: What Level of Care is Best for My Wife?
Dear Rae:
I feel completely helpless. My wife has been drinking heavily for years, but she has a good job and is very active. She runs three times a week and we have a pretty big social life. Here’s the problem – lately, she seems to be drinking more and it is impacting her quality of life (and mine). There have been a couple “incidents” at parties and she seems to be making excuses to not do things she used to do – she gets drunk more often and faster.
I have found a small vodka bottle hidden in her desk drawer at home (yes I am snooping around because I’m worried). I do not know what to do next. What are the options for rehab? Does she have to go away for a month? Any advice is welcome. D W
Dear D W:
First, there are many options for addiction treatment. From education classes to a residential stay. And it sounds like you need help to determine what level of therapeutic support is appropriate for your wife, while being mindful of what suits your lifestyle. Our admissions counselors will make recommendations, but the ultimate choice is for both you and your wife to consider.
Calling Admissions to Discuss Level of Care…
Our skilled admissions counselors are available to answer questions, provide a screening to determine the best course of action, or just chat. But a phone screening will determine what level of care is recommended. Phone screening answers the following questions:
- How much and how often a person is using their drug of choice
- Support system and family environment
- Insurance coverage
- Whether a stay in sub-acute detox is necessary
- Level of care recommended – Residential, Outpatient (PHP, IOP) Programs
You ask about whether a 30 day stay in a residential facility is necessary. It is not necessary or appropriate in every case. Keep in mind however, that a stay in a comfortable, controlled environment (away from the people, places and things that trigger alcohol use) is often the most effective way to galvanize the recovery process.
Outpatient programs are available at different levels, with varying time commitments. This allows for treatment after work or during the day while living at home. There are also education and relapse prevention classes available after a period of sobriety.
Biophychosocial Assessment
No matter what program is chosen, a biophychosocial assessment is done by a master’s level therapist in coordination with medical staff. The biophychosocial approach systematically evaluates the interactions between the biological, psychological and social factors in understanding health, illness and health care delivery.
One-on-one therapy and family therapy are also vital components to long term success in recovery. And choosing a treatment facility with a full spectrum of addiction treatment options will allow you more flexibility – especially with a busy lifestyle.
Have you talked to your wife about this?
Ideally, you will find a quiet time to talk to your wife about your concerns. Know that if you are sensing a problem, it is likely that some level of support and/or treatment is appropriate. It is best if your wife is involved in the decision to seek help and a participant in the call to Admissions. Make sure she understands there is no obligation. It;s just a phone call. But make the call. It is a huge first step in the right direction.

Dear Rae: Is My 15-Year Old Using Alcohol & Drugs?
Dear Rae:
My teenage son has begun to worry my husband and me. He is sullen and non-communicative – which is very new behavior in our house. We are a close family and he is our only child. In the past, John was open about school, friends and outside activities. But recently, he has been secretive – one-word answers to questions and snapping at us when we try to talk to him. He also says he wants to quit soccer next year – it has been his favorite sport since first grade…
I would pass it off as typical “teenage behavior”, but he has also seemed out of it when he comes home from an overnight at a friend’s house. And I swear I have smelled alcohol on his breath. I am frankly scared to confront him for fear he will close down even more. He and his friends have never given us cause to worry. Should I give it some time or search his room? Confront him? Hide the alcohol in the house? My husband and I drink.
KL
Dear KL:
First, if you are concerned about John’s behavior, you need to talk to him. There is a reason you have that “feeling” in the pit of your gut. It is easy in this busy world to let things fester or feel disconnected with loved ones. Establish dependable times to be together – dinnertime, or first thing in the morning when you can get a good benchmark on his behavior and general mental and psychical health. And never let things go – with teenagers there will be conflict. Try not to be afraid of confrontation – and speak without anger or accusation.
The facts are indisputable. According to the CDC, approximately 30% of high school students drink alcohol and about half of those binge drink. In West Michigan, the average age of first use of alcohol and other drugs is 13. The negative ramifications include introduction to other drugs and dangerous behaviors while under the influence. And the impact on brain development could have life-long effects.
Talk to your son.
Before you start searching his room, talk to your son. Allow him a “safe place” to express honestly. If there is alcohol in the home, this could present an opportunity to talk about why the legal age for drinking is 21 and the vulnerabilities associated with early use. Follow your parental instinct. If the behavior continues, seek help/guidance through a professional with a specialty in adolescent behavior or a local support group.
What you are asking is important. Don’t underestimate the impact of early use on your son. Statistics tell us that 9 out of 10 people who struggle with substance use started using before the age of 21. A good first place to educate yourself is online with the Substance Abuse & Mental Health Services Administration (SAMSHA) Parent Resources .
Rae Green
Dear Rae: I want my fiftieth year to be my healthiest and soberest…
Dear H:
Cheers to 50!
Dear Rae: I have a friend I am very concerned about…
… During the week she holds down a very good job, works out regularly, cooks healthy meals for herself, and even spends time volunteering. She appears enviably happy.
As soon as the weekend hits…
As soon as the weekend hits, however, it is like a different person emerges. She often combines prescription medications with alcohol causing her to black out. She often drinks the next day to ease her hangover. I have picked her up from strangers’ houses, bars, and even random street corners only to have her wake up on my couch the next morning with scant memories of the night before. She has very few friends that will go out with her because it inevitably turns into babysitting a belligerent, foul mouthed, 30 year old. I’ve tried several times to approach her with my concerns, only to be shot down and reminded of her weekday successes. She believes that because she\’s sober 5 nights out of the week that she doesn’t have a problem, but her binging is out of control. Lauren
Dear Lauren:
Let’s start with the weekend and work backwards. A blackout is caused by drinking a large amount of alcohol in a short period of time. Your friend may abstain during the week, but she is exhibiting dangerous behavior on the weekends. Binging and mixing alcohol and prescription medications, blacking out and drinking to lessen a hangover are all symptoms of the disease of alcoholism. If your friend continues on this narrowing path, she will eventually lose her ability to control herself during the week.
I am going to say something you may not want to hear… When you pick her up from compromising situations, allow her to crash on your couch and rationalize her behavior, you are allowing the negative behavior to continue. I know how difficult it is to approach someone you care about, to talk about their drinking problem. But the issue is not how often your friend drinks (although weekend binges are problematic). It’s the fact that her drinking is causing problems in her personal life that she is unwilling to address. Even if they only occur on the weekends.
The components of life are varied – work, interpersonal relationships, physical health…Your friend’s most visible activities are managed, but her personal life, safety and health are being impacted. In addiction, social, occupational and recreational activities are neglected or abandoned. It is almost certain that, even though she says her life is not impacted by alcohol during the week, her weekend behavior is spilling over into her weekdays. How do you think she feels on Monday mornings? How productive do you think she is on Friday afternoons?
The best thing you can do, is to sit her down and tell her that you care about her and want to remain her friend, but not while she’s drinking. Rae
Dear Rae, I have been sober for a little over a year now. I have been struggling the past few weeks and recently had an alcoholic beverage, my first since I gave up drinking last year. My friend Albert says that I have relapsed, even though I haven’t had another drink since. Is he right? – Rob C.
Dear Rob: I would say this is a lapse, not a relapse. It’s like you sprained your ankle, instead of completely breaking your leg. But, a “relapse” and a “lapse” are as much about functioning and thinking, as they are about using alcohol. Taking a sip of alcohol is not the lapse. That’s the end result of addictive thinking. A relapse begins psychologically. The sipping of the alcohol is just the visual of other things that have been going on. These “struggles” are important to address from this day forward.
Don’t Focus on the Relapse…
Don’t focus on the relapse, it’s just a word. You can tell that to your friend Albert… Your concern and priority should be getting back on track immediately.
An important thing to note, is that you knew you had been “struggling”. Make sure you’re actively practicing your recovery. When you become complacent, addictive thinking can start to creep in. Think about what stressors and triggers led you to that drink and be mindful of those in the future. Know that there are signs like, mood swings that you and others can watch for in order to prevent a lapse.
Use this as a learning experience. Put what you learned into your recovery tool kit to make you stronger and smarter. Your next step is to address how you are going to move forward. Be aware. If you begin to struggle again, talk to a sober friend, step up your 12-step meeting schedule or get out and get some exercise. If the difficulties continue, seek professional help.
Rae
Ask Rae: How do I manage my recovery during the upcoming holiday season? – Emily
Dear Emily:
The holidays are meant to be a time for joy and merriment. But, for a lot of people holidays bring stress, whether it’s from being around family members to traveling. The holiday season is especially challenging and stressful for people in recovery. There are cocktail parties (even the name is triggering) and heavy drinking gatherings that can bring about strong urges. BUT, you don’t need old substances to have a festive time. There are some proactive steps you can take to reduce your stress and keep moving forward in your recovery.
You can bump up your support system. During the holidays, reach out to your sponsor, therapist, and support group more frequently. Spend time with others in recovery. Your support system can help you recognize your personal limits. You can talk with them before you go to that holiday party and then plan to meet with them afterwards.
If you are going to a party where there will be alcohol or other substances, evaluate the situation and have a plan in advance. Bring a sober friend with you. Drive yourself, so you have a way to leave the party and go someplace safe if needs be. In addition, you can make sure to arrive early and leave early to avoid prolonged exposure. Or, you can set a time frame beforehand and clearly state it when you arrive. Then stick to it.
Prepare responses and rehearse them. If you’re not ready to share about your recovery with family and friends, have a strategy for turning down drinks or other substances, as this is when vulnerability is at its peak.
Know your triggers and how to manage them. Take care of your mental and physical health. Be sure to take some quiet time each day. Fit relaxation and meditation into your day, if just for a few minutes, no matter how busy you are. Get enough sleep every night too. Eat nutritious meals or a snack every few hours to keep your blood sugar up. Low blood sugar can make you feel anxious or irritable making you feel impulsive or tempted. If you’re early in recovery, stay in low risk situations and avoid ones that are high risk. If further along in recovery, know your plan for when you’ll be in a medium or high risk.
Celebrate the season in a new way. Create new rituals or symbols that help redefine joy for you in your recovery during the holidays. You can host your own holiday party for recovery friends or your support group.
Rae
Dear Rae: How can my family play a positive role in my treatment & recovery? K.B.
Dear KB: I’m glad you asked this question. It is critical the entire family be educated about the disease of addiction. Education and family therapy will support your treatment and recovery. Members of the family system often refuse to acknowledge their role. We want to make family members allies and partners in the recovery process. With therapy and education, we are able to deal with the potential for blame – for your past behavior or your continuing behavior.
We want to manage your family’s expectations. It is unrealistic to assume you are “fixed” when you leave treatment. But it is natural for your family to think you will feel better immediately. Without education, family members are unaware of Post-Acute Withdrawal (PAWs) symptoms. PAWs can make someone new to recovery tired, edgy, sleep deprived and out of sorts. The symptoms of PAWs can last up to three years. When we involve the family in the recovery process, they begin to understand the path of the disease, the root cause of addiction and their role and responsibilities in the recovery plan.
Dear Rae: I relapsed, how do I move forward? Stymied
Dear Stymied: As with many other progressive, chronic illnesses, relapse is unfortunately part of the recovery process. It reminds me of going off a diet to eat a cookie and then thinking “the damage is done, might as well eat the whole box.” In treatment we teach that the tools to address the relapse are just as important as the tools to prevent it. So not only do you learn how to prevent yourself from giving into that craving, you learn how to address the situation when you’ve given in and are two boxes of thin mints deep. The way to move forward is to work through the shame and guilt. Reach out for help. Rely on your support systems (that are hopefully already put in place). For more insight about relapse check out the blog post 10 Triggers to Relapse/10 Practical Sober Solutions and 7 Ways to Stop Fearing Relapse.
Dear Rae: I want to go to residential treatment but I don’t want to leave my kids. Will I be able to see them in my time away? Miserable Mama
Dear MM: Sanford House is a women’s addiction treatment center. We are well aware that many of the women who come to us are moms. The fact is, when you’re deep in your addiction, you’re not present as a caretaker. So time spent in treatment, is necessary to begin the healing process. In the long run, being away from your kids during treatment can be valuable to your recovery. At Sanford House, we support communications between our women residents and their families. Daily phone calls and skype or facetime chats are allowed and family therapy sessions are provided and encouraged. Addiction is a family disease and we know your relationship with your children is vital to your good health and successful recovery.
Dear Rae: If I go to detox, do I still need to go to treatment? B.
Dear B: The purpose of detox is to rid the body of alcohol or drugs in a physically safe way. But detox is not addiction treatment or rehab. In the simplest sense, detox deals with the physical aspects of addiction. Treatment deals with the emotional aspects, like the emotional pain of substance abuse. So, the answer to your question is, “Yes.” If you’d like more information, I’ve written an article called “What is Drug and Alcohol Detox“